| Content | Secondary rhinoplasty surgery, or in other words, revision rhinoplasty surgery is the reoperation of a person who has undergone nose surgery due to an aesthetic or functional defect that cannot be corrected despite surgery or that occurs after surgery. This surgery can also be called secondary nose surgery.
With the second operation, additional procedures such as intervention in more than one area of the nose and the use of cartilage grafts may be required.
When Can Secondary Rhinoplasty Surgery Be Performed?
In order for the secondary nose surgery to be performed, at least 1 year must pass after the first nose surgery. This period is important for the nose to regain its natural state after surgery. Otherwise, the success rate of the second nose surgery will decrease.
How is Secondary Rhinoplasty Performed?
It is necessary to take cartilage for the second nose surgery and if there is not enough cartilage in the nose, it may be necessary to take cartilage from the patient's ear or rib region. Since all cartilages are usually removed during the first surgery, the use of cartilages in the ear and rib region is quite common. |
| INPATIENT MEN V.I.P. CHECK-UP |
| LABORATORY ANALYSIS |
| Glucose |
To determine whether or not your blood glucose level is within normal ranges; to screen for, diagnose, and monitor diabetes, and to monitor for the presence of hypoglycaemia (low blood glucose) and hyperglycaemia (high blood glucose) |
| HbA1c |
To monitor average blood glucose levels over a 3 month period. Used to help diagnose and monitor people
with diabetes. |
| Urea (Bun) |
To measure how much of waste product you have in your blood. It is used to determine how well your kidneys
are working |
| Creatinine |
To assess kidney functions |
| Uric Acid |
To diagnose kidney disorder,diagnose and monitor people with gout, monitor kidney function. |
| Complete Urinalysis Test |
To look for metabolic and/or kidney disorders and for urinary tract infections |
| Total Cholesterol |
To screen for risk of developing cardiovascular disease (heart disease, stroke and related diseases); to monitor treatment |
| LDL Cholesterol |
| HDL Cholesterol |
| Triglycerides |
| AST (SGOT) |
To diagnose liver, bile duct and heart diseases. |
| ALT (SGPT) |
| GGT |
To screen for liver disease or alcohol abuse; and to help your doctor tell whether a raised concentration
of alkaline phosphatase (ALP) in the bloodstream is due to liver or bone disease |
| ALP |
To screen for or monitor treatment for liver or bone disorder |
| Sodium |
To investigate causes of dehydration, oedema, problems with blood pressure, or non-specific symptoms |
| Potassium |
To help diagnose and determine the cause of an electrolyte imbalance; to monitor treatment for illnesses that
can cause abnormal potassium levels in the body |
| Chloride |
To determine if there is a problem with your body’s acid-alkali (pH) balance and to monitor treatment |
| Calcium |
To scan, diagnose, and monitor a range of conditions relating to the bones, heart, nerves, kidneys, and teeth. |
| Phosphate |
To help in the diagnosis of conditions known to cause abnormally high or low levels |
| Amylase |
To diagnose pancreatitis or other pancreatic diseases |
| Lipase |
To diagnose and monitor pancreatitis or other pancreatic disease |
| Magnesium |
To measure the concentration of magnesium in your blood and to help determine the cause of
abnormal calcium and/or potassium levels |
| C-Reactive Protein (CRP) |
To identify the presence of inflammation, to determine its severity, and to monitor response to treatment. |
| 25 Hydroxy Vitamin D |
To investigate a problem related to bone metabolism or parathyroid function, possible vitamin D deficiency, malabsorption, before commencing specific bone treatment and to monitor some patients taking vitamin D. |
| RF (Rheumatoid Factor) |
To help diagnose rheumatoid arthritis (RA) and Sjögren’s syndrome |
| Albumin |
To screen for liver or kidney disease especially in hospitalised patients |
| aPTT |
A part of investigation for bleeding or thrombotic episode |
| Blood Count Haemogram |
Haemogram serves as broad screening panel that checks for the presence of any diseases and infections in the
body. |
| Erythrocyte Sedimentation Rate
(ESR) |
To detect and monitor the activity of inflammation as an aid in the diagnosis of the underlying cause |
| Ferritine |
To help assess the levels of iron stored in your body |
| Vitamin B12 |
To help diagnose the cause of anaemia or neuropathy (nerve damage), to evaluate nutritional status in some
patients, to monitor effectiveness of treatment of B12 or folate deficiency |
| Free T4 |
To diagnose hypothyroidism or hyperthyroidism in adults and to monitor response to treatment |
| TSH |
To screen for and diagnose thyroid disorders; to monitor treatment of hypothyroidism and hyperthyroidism |
| Folate |
A cause of anemia or neuropathy; to evaluate nutritional status in some people; to monitor the effectiveness of
treatment for vitamin B12 or deficiency |
| Testosterone |
To find out if testosterone levels are abnormal in patients |
| HBsAg |
To detect, diagnose and follow the course of an infection with hepatitis B virus (HBV) or to determine if
the vaccine against hepatitis B has produced the desired level of immunity |
| Anti HCV |
To screen for and diagnose hepatitis C virus infection and to monitor treatment of the infection |
| Anti HIV |
To determine if you are infected with human immunodeficiency virus (HIV) |
| CEA |
In the presence of certain cancers, CEA may be used to monitor the effect of treatment and recurrence of
disease |
| CA19-9 |
To help tell the difference between cancer of the pancreas and bile ducts and other conditions; to monitor
response to pancreatic cancer treatment and to watch for recurrence. |
| AFP |
To screen for and monitor therapy for certain cancers of the liver and testes |
| Total PSA |
To help detect and to monitor prostate cancer |
| Fecal Occult Blood Test |
To screen for bleeding from the gut/intestine, which may be an indicator of bowel cancer |
| Helicobakter Pylori Antigen In
Feces |
To diagnose an infection with Helicobacter pylori (H. pylori), the bacteria that can cause peptic ulcers; to determine whether treatment has cured the infection |
| Feces Microscopy (Stool Culture) |
To determine whether you have an infection of your digestive tract due to the presence of disease-causing (pathogenic) bacteria |
| OTHER ANALYSIS |
| White Blood Cell Count |
To screen for or diagnose a variety of conditions that can affect the number of white blood cells (WBCs), such
as an infection, inflammation or a disease |
| Coronary CT Angiography |
It is a imaging method performed by computed tomography of the coronary arteries, which are the vessels
that feed the heart, by giving contrast material through the vein of the forearm. |
| Abdominal Ultrasound |
To identify diseases at organs in the abdomen, including the liver, gallbladder, spleen, pancreas, and kidneys. |
| Thyroid Ultrasound |
To characterize a thyroid nodule(s), i.e. to measure the dimensions accurately and to identify internal structure
and vascularization |
| Carotid Ultrasound |
To detect narrowing, or stenosis, of the carotid artery, a condition that substantially increases the risk of stroke |
| Chest X-Ray |
The most commonly preferred diagnostic examination to produce images of heart, lungs, airways, blood
vessels and the bones of the spine and chest |
| Electrocardiogram |
To measure the electrical activity of the heartbeat and hearth rhythm |
| Exercise Stress Test |
To determine how well your hearth handles work. The test can show if the blood supply is reduced in the
arteries that supply the heart |
| Eco Doppler + Color + M Mode + B
Mode |
|
| Holter Monitoring |
To track your hearth's rhythm for 24 hours |
| Ambulatory Blood Pressure
Monitoring |
To measure your blood pressure for 24 hours |
| Uroflowmetry |
To measure of the rate of urine flow over time |
| Addenbrooke Cognitive
Evaluation |
|
| Gastroscopy |
To test that looks at the inside of your food pipe (oesophagus), stomach and the first part of your small
intestine (small bowel). |
| Colonoscopy |
To look at the whole of the inside of the large bowel to check the bowel routine and help find the cause of
symptoms of bowel |
| EXAMINATIONS |
| Internal Medicine Examination |
General physical examination, evaluation of the results and recommendations. |
| Cardiology Examination |
| General Surgery Examination |
| Urology Examination |
| Ophtalmology Examination |
| Neurology Examination |
| Psychological Interview |
| Nutritionist And Dietican |
|
Breast Health Package for Women Over 40
Our Breast Health Center, which is a part of Yaşam Hospital Oncology Center, offers all the possibilities of technology to provide the best care to every woman.
What is Mammography?
Mammography is the low-dose X-ray imaging of the breast tissue to look for early signs of breast cancer before symptoms develop. It can also be used for due diligence when a new symptom (lump or focal pain) develops in the breast tissue.
When viewed on a mammogram, breast tissue appears white and opaque (nebula), while fatty tissue appears darker and translucent.
When Should a Mammogram Be Done?
Annual screening mammograms are recommended for all women from the age of 40. Women who do not have any breast-related signs or symptoms are also screened. If an abnormality is present or patients have a new symptom (a lump or focal pain), additional evaluation may be required. Further examination will reveal what these suspected abnormalities are.
What Percent of Women Who Have Had Mammography Have Risky Situations?
Potential abnormalities are found in 6 to 8 percent of women who get mammograms. This group undergoes different additional evaluations, which may include breast physical examination, diagnostic mammography, breast ultrasound or needle biopsy.After these additional evaluations are completed, it becomes clear what the abnormalities found on the mammogram are.
What Does an Abnormality Look Like on a Mammogram?
The possible abnormality on a mammogram may be called a nodule, mass, lump, density or deterioration:
A mass (lump) with a smooth, well-defined border is usually benign.
Ultrasound is necessary to see and identify the inside of a mass. If the mass contains fluid, it is called a cyst.
A mass (lump) with irregular borders or a starburst appearance may be cancerous and a biopsy is usually recommended.
Microcalcifications (small calcium deposits) are another type of abnormality. They can be classified as benign, suspicious, or uncertain. Most microcalcifications are benign. Depending on how the microcalcifications appear in additional studies (magnification views), a biopsy may be recommended.
What is the Accuracy Rate of Mammography?
Diagnoses made by mammography are between 85 percent and 90 percent accurate. Mammograms can detect breast abnormalities before they are large enough to be felt. However, a palpable mass may not be seen on a mammogram. Any abnormality you feel while examining your breasts should be evaluated by your doctor.
What Should Be Considered Before Mammography?
You can follow your normal routine before the mammogram. You can take your medications and maintain your eating and drinking patterns. If you are breastfeeding, pregnant or think you may be pregnant, you should tell your doctor as your mammogram may need to be postponed.
What Should I Pay Attention to When Coming to My Mammography Appointment?
The technician will ask you to remove one breast from your bib at a time and place it on the chest support plate. The image of the breast is taken by clamping it between two plates. In the meantime, pressure is applied to the breast, preventing the breast from moving. This pressure spreads the breast tissue, allowing the radiologist to see the tissue better. Also, the least amount of radiation is used when the breast is compressed as finely as possible.
You may feel some discomfort during 3-5 seconds of pressure. If you cannot tolerate the pressure, please let the technician know. Pressure can be more bothersome at some times in a woman’s menstrual cycle. To minimize discomfort, we recommend scheduling your appointment seven to 10 days after the start of your period.
How is a Mammogram Taken?
The technician will ask you to remove one breast from your bib at a time and place it on the chest support plate. The image of the breast is taken by clamping it between two plates. In the meantime, pressure is applied to the breast, preventing the breast from moving. This pressure spreads the breast tissue, allowing the radiologist to see the tissue better. Also, the least amount of radiation is used when the breast is compressed as finely as possible.
You may feel some discomfort during 3-5 seconds of pressure. If you cannot tolerate the pressure, please let the technician know. Pressure can be more bothersome at some times in a woman’s menstrual cycle. To minimize discomfort, we recommend scheduling your appointment seven to 10 days after the start of your period.
How Does the Process Proceed After Mammography?
There may be temporary skin discoloration and/or mild pain in the chest due to compression. Most women will be able to resume their normal activities soon after their mammogram. Your results will be available within a few days after the test. After getting the results, your doctor will explain everything to you.
How Often Should You Have a Mammogram?
Regular mammograms every year, starting at the age of 40, will enable you to recognize potential risks early.
What Does the Breast Health Package Consist of?
Breast health package consists of General Surgery Examination and Mammography |
| GENERAL CARDIOLOGY SCREENING PACKAGE |
| LABORATORY ANALYSIS |
| Glucose |
To determine whether or not your blood glucose level is within normal ranges; to screen for, diagnose, and monitor diabetes, and to monitor for the presence of hypoglycaemia (low blood glucose) and hyperglycaemia (high blood glucose) |
| HbA1c |
To monitor average blood glucose levels over a 3 month period. Used to help diagnose and monitor people with diabetes |
| Urea (Bun) |
To measure how much of waste product you have in your blood. It is used to determine how well your kidneys are working |
| Creatinine |
To assess kidney functions |
| Uric Acid |
To diagnose kidney disorder,diagnose and monitor people with gout, monitor kidney function |
| Complete Urinalysis Test |
To look for metabolic and/or kidney disorders and for urinary tract infections |
| Total Cholesterol |
To screen for risk of developing cardiovascular disease (heart disease, stroke and related diseases); to monitor treatment |
| LDL Cholesterol |
| HDL Cholesterol |
| Triglycerides |
| AST (SGOT) |
To diagnose liver, bile duct and heart diseases |
| ALT (SGPT) |
| Sodium |
To investigate causes of dehydration, oedema, problems with blood pressure, or non-specific symptoms |
| Potassium |
To help diagnose and determine the cause of an electrolyte imbalance; to monitor treatment for illnesses that can cause abnormal potassium levels in the body |
| Calcium |
To scan, diagnose, and monitor a range of conditions relating to the bones, heart, nerves, kidneys, and teeth |
| C-Reactive Protein (CRP) |
To identify the presence of inflammation, to determine its severity, and to monitor response to treatment |
| 25 Hydroxy Vitamin D |
To investigate a problem related to bone metabolism or parathyroid function, possible vitamin D deficiency, malabsorption, before commencing specific bone treatment and to monitor some patients taking vitamin D |
| Homocysteine |
To find out if you are at high risk of a heart attack or stroke; also used to determine if you are folate-deficient or vitamin B12-deficient |
| Lipoprotein A |
To evaluate targeted screening for cardiovascular disease (coronary artery disease (CAD) and cerebrovascular disease) risk assessment |
| Blood Count Haemogram |
Haemogram serves as broad screening panel that checks for the presence of any diseases and infections in the body. |
| Troponin |
To see if you have had a heart attack or damage to your heart muscle |
| Vitamin B12 |
To help diagnose the cause of anaemia or neuropathy (nerve damage), to evaluate nutritional status in some
patients, to monitor effectiveness of treatment of B12 or folate deficiency |
| Free T3 |
To help diagnose hyperthyroidism and monitor it's treatment |
| Free T4 |
To diagnose hypothyroidism or hyperthyroidism in adults and to monitor response to treatment |
| TSH |
To screen for and diagnose thyroid disorders; to monitor treatment of hypothyroidism and hyperthyroidism |
| D- dimer |
To help diagnose or exclude thrombotic (blood clot producing) or bleeding diseases and conditions |
| OTHER ANALYSIS |
| Carotid Ultrasound |
To detect narrowing, or stenosis, of the carotid artery, a condition that substantially increases the risk of stroke |
| Echocardiogram |
To evaluate how your heart moves, heart valves are working and heart’s pumping strength |
| Electrocardiogram |
To measure the electrical activity of the heartbeat and hearth rhythm |
| Exercise Stress Test |
To determine how well your hearth handles work. The test can show if the blood supply is reduced in the arteries that supply the heart |
| EXAMINATIONS |
| Cardiology Examination |
General physical examination, evaluation of the results and recommendations |
| General Surgery Examination |
| Dermatology Examination |
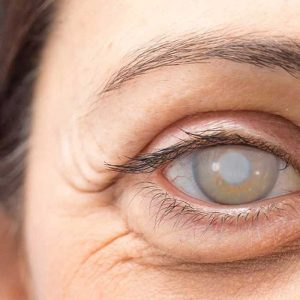
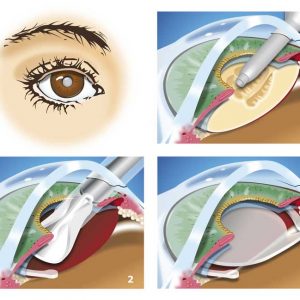
| Blepharoplasty is the general name of the aesthetic corrections we make on the eyelid. Eyelid aesthetics is one of the most common surgical fields of oculoplastic surgery.
Excess skin on the upper eyelid, weakness in the muscle and connective tissue under the skin, collapses in the adipose tissue, sagging of the lacrimal gland; Sagging of the lower eyelid, excess skin, collapsed areas between the lid and cheek, and weakness in the lower lid can be removed by blepharoplasty operations.
The important thing here is to determine which of the above-mentioned procedures will be required by a detailed examination and to plan the surgery that is suitable for the patient meticulously. |
| OVERALL CARDIOLOGY SCREENING PACKAGE |
| LABORATORY ANALYSIS
|
| Glucose |
To determine whether or not your blood glucose level is within normal ranges; to screen for, diagnose, and monitor diabetes, and to monitor for the presence of hypoglycaemia (low blood glucose) and hyperglycaemia (high blood glucose) |
| HbA1c |
To monitor average blood glucose levels over a 3 month period. Used to help diagnose and monitor people with diabetes. |
| Urea (Bun) |
To measure how much of waste product you have in your blood. It is used to determine how well your kidneys are working |
| Creatinine |
To assess kidney functions |
| Uric Acid |
To diagnose kidney disorder,diagnose and monitor people with gout, monitor kidney function. |
| Complete Urinalysis Test |
To look for metabolic and/or kidney disorders and for urinary tract infections |
| Total Cholesterol |
To screen for risk of developing cardiovascular disease (heart disease, stroke and related diseases); to monitor treatment |
| LDL Cholesterol |
| HDL Cholesterol |
| Triglycerides |
| AST (SGOT) |
To diagnose liver, bile duct and heart diseases. |
| ALT (SGPT) |
| Sodium |
To investigate causes of dehydration, oedema, problems with blood pressure, or non-specific symptoms |
| Potassium |
To help diagnose and determine the cause of an electrolyte imbalance; to monitor treatment for illnesses that can cause abnormal potassium levels in the body |
| Calcium |
To scan, diagnose, and monitor a range of conditions relating to the bones, heart, nerves, kidneys, and teeth |
| C-Reactive Protein (CRP) |
To identify the presence of inflammation, to determine its severity, and to monitor response to treatment |
| 25 Hydroxy Vitamin D |
To investigate a problem related to bone metabolism or parathyroid function, possible vitamin D deficiency, malabsorption, before commencing specific bone treatment and to monitor some patients taking vitamin D |
| Homocysteine |
To find out if you are at high risk of a heart attack or stroke; also used to determine if you are folate-deficient or vitamin B12-deficient |
| Lipoprotein A |
To evaluate targeted screening for cardiovascular disease (coronary artery disease (CAD) and cerebrovascular disease) risk assessment |
| Blood Count Haemogram |
Haemogram serves as broad screening panel that checks for the presence of any diseases and infections in the body. |
| Troponin |
To see if you have had a heart attack or damage to your heart muscle |
| Vitamin B12 |
To help diagnose the cause of anaemia or neuropathy (nerve damage), to evaluate nutritional status in some patients, to monitor effectiveness of treatment of B12 or folate deficiency |
| Free T3 |
To help diagnose hyperthyroidism and monitor it's treatment |
| Free T4 |
To diagnose hypothyroidism or hyperthyroidism in adults and to monitor response to treatment |
| TSH |
To screen for and diagnose thyroid disorders; to monitor treatment of hypothyroidism and hyperthyroidism |
| D- dimer |
To help diagnose or exclude thrombotic (blood clot producing) or bleeding diseases and conditions |
| OTHER ANALYSIS |
| Carotid Ultrasound |
To detect narrowing, or stenosis, of the carotid artery, a condition that substantially increases the risk of stroke |
| Echocardiogram |
To evaluate how your heart moves, heart valves are working and heart’s pumping strength |
| Electrocardiogram |
To measure the electrical activity of the heartbeat and hearth rhythm |
| Coronary CT Angiography |
It is a imaging method performed by computed tomography of the coronary arteries, which are the vessels that feed the heart, by giving contrast material through the vein of the forearm |
| EXAMINATIONS |
| Cardiology Examination |
General physical examination, evaluation of the results and recommendations |
| General Surgery Examination |
| Dermatology Examination |
| OTHER ANALYSIS |
| Carotid Ultrasound |
To detect narrowing, or stenosis, of the carotid artery, a condition that substantially increases the risk of stroke |
| Echocardiogram |
To evaluate how your heart moves, heart valves are working and heart’s pumping strength |
| Electrocardiogram |
To measure the electrical activity of the heartbeat and hearth rhythm |
| Coronary CT Angiography |
It is a imaging method performed by computed tomography of the coronary arteries, which are the vessels that feed the heart, by giving contrast material through the vein of the forearm |
| EXAMINATIONS |
| Cardiology Examination |
General physical examination, evaluation of the results and recommendations |
| General Surgery Examination |
| Dermatology Examination |
|

























Reviews
There are no reviews yet.